Friend or Foe?
Let’s Untangle the Advice
Hey everyone, and welcome back to our IBS Awareness Month series!
Last time, we explored the what, why, and how of IBS. This week, we’re diving into a topic that causes a lot of confusion (and maybe even some anxiety) for those living with Irritable Bowel Syndrome: fibre.
You’ve probably heard it all, right? “Eat more fibre!” But then maybe you tried that… and instead of feeling better, you were hit with more bloating, gas, pain, or even found yourself running to the bathroom – or feeling more backed up. So frustrating!
Does it feel like the one thing everyone says is healthy is actually making your IBS worse?
So, what’s the truth? Is fibre a friend or foe when you have IBS? Like most things with IBS, it depends. But once you understand why, you can navigate it with more confidence.
Let’s break it down.

First Up: What Exactly Is Fibre?
Think of fibre as the tough, structural part of plant foods (fruits, veggies, grains, legumes, nuts, seeds) that your body can’t actually digest or absorb. It travels through your digestive system relatively intact.
Then Why Do We Even Need It?
Even if it feels tricky for your gut right now, fibre plays some crucial roles for overall health:
- Keeps You Regular: Adds bulk and supports healthy bowel movements, either speeding things up or slowing them down, depending on the type.
- Feeds Your Gut Microbiome: Some fibres are prebiotics, which help nourish the beneficial bacteria in your large intestine.
- Supports Heart Health & Blood Sugar Control: Fibre can help lower cholesterol and slow sugar absorption.
- Helps with Satiety: It keeps you feeling full longer, which can be helpful for appetite regulation and weight management.
How Much Fibre Are We “Supposed” To Have?
General recommendations suggest aiming for:
- Women (19–50): 25 grams per day
- Women (>50): 21 grams per day
- Men (19–50): 38 grams per day
- Men (>50): 30 grams per day
But wait – if you have IBS, looking at those numbers might feel overwhelming. Don’t panic. These are general population guidelines. Your personal tolerance and needs may be very different, and that’s okay.
The IBS Twist: Why Fibre Gets Complicated
Here’s where it gets personal. While fibre is beneficial in general, how it behaves in your sensitive gut is key. The main reason fibre can trigger IBS symptoms comes down to two factors:
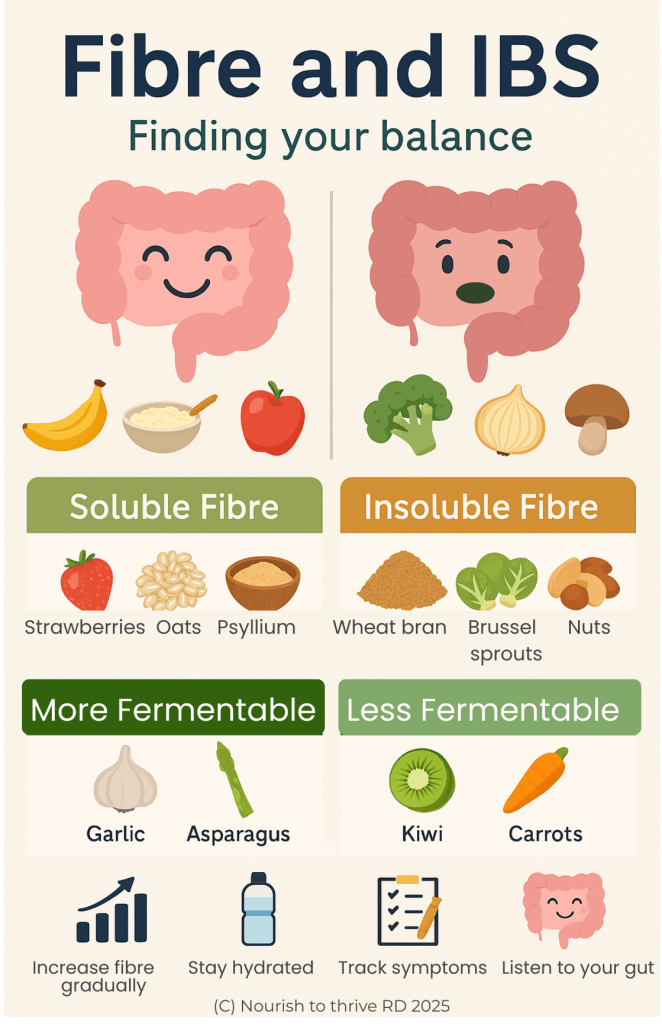
1. The Type of Fibre
- Soluble Fibre: Dissolves in water, forming a gel. It is found in oats, barley, psyllium husk, beans, apples, citrus fruits. It can generally help both diarrhea (by absorbing water) and constipation (by softening stool).
- Insoluble Fibre: Doesn’t dissolve in water. Adds bulk and speeds things along. It is found in wheat bran, whole grains, nuts, seeds, and the skins of fruits and veggies. Helpful for some, irritating for others.
2. Fermentation: The IBS Wildcard
Remember those beneficial gut bacteria? They love to ferment certain foods and fibres (like inulin, found in chicory root). One of the major byproducts of their fermentation feast? Gas!
For someone without IBS, a bit of gas is no big deal. But for people with IBS, the gut is often hypersensitive (visceral hypersensitivity):
- Normal gas feels painful because the gut nerves are more sensitive.
- Gas might move slower due to motility issues, leading to trapped gas, bloating, and discomfort.
It’s also worth noting that some carbohydrates – known as FODMAPs – can ferment even more rapidly than fibre, often triggering more intense symptoms in those with IBS such as bloating, distension (visible belly swelling), and abdominal pain.
While these can still offer health benefits when included as tolerated, FODMAPs are a unique category that deserves its own spotlight (stay tuned – more on that in an upcoming post!).
Another fascinating by-product of fermentation is short-chain fatty acids (SCFAs). These compounds are known to offer a range of health benefits, such as regulating appetite and protecting and nourishing the gut lining. More on SCFAs in a future post!
To summarize, fibre is a key component of a healthy, well-balanced diet and does not need to be overly-restricted for most people with IBS. Since individual tolerance varies, consulting a registered dietitian is recommended to find that perfect balance.
Starting Points for Your Fibre Journey
Here are some general principles to guide your IBS-fibre exploration:
- Make Changes Slowly: Whether you’re adding, removing, or swapping fibre sources, gradual adjustments are usually better tolerated by sensitive guts.
- Know Your Fibre Types: Start identifying which fibres are soluble, insoluble, and fermentable. Understanding this can help you make informed swaps.
- Stay Hydrated: Water helps fibre do its job effectively. Always prioritize hydration.
- Track Your Symptoms: Paying attention to how your body responds after eating different foods and fibre amounts can provide valuable personal insights over time.
- Respect Your Body’s Limits: Your fibre needs and tolerance may be different from others. That’s okay! This is about your unique balance.
Finding Your Fibre Balance Takes Time
Navigating fibre with IBS is a journey of trial, error, and self-discovery. It’s okay if your current intake doesn’t match the guidelines. The goal is to find a balance that supports your gut health without triggering symptoms.
Understanding why certain fibres can cause issues (hint: fermentable or insoluble!) can be the first step toward more confident, informed choices.
Feeling Lost in the Fibre Maze?
Trying to figure out fibre types, fermentability, FODMAPs, and your personal tolerance alone can feel overwhelming. You don’t have to do it alone.
Working with a registered dietitian can help you:
- Identify your specific fibre triggers
- Develop a personalized plan to add in tolerable fibres
- Navigate the Low FODMAP diet (if appropriate)
- Ensure you’re meeting your nutrition needs while managing symptoms
Ready to get personalized support?
Click here to book a free discovery call to see how we can work together to find your unique fibre balance!
Don’t let fibre confusion hold you back. Take the next step toward understanding your gut better!
